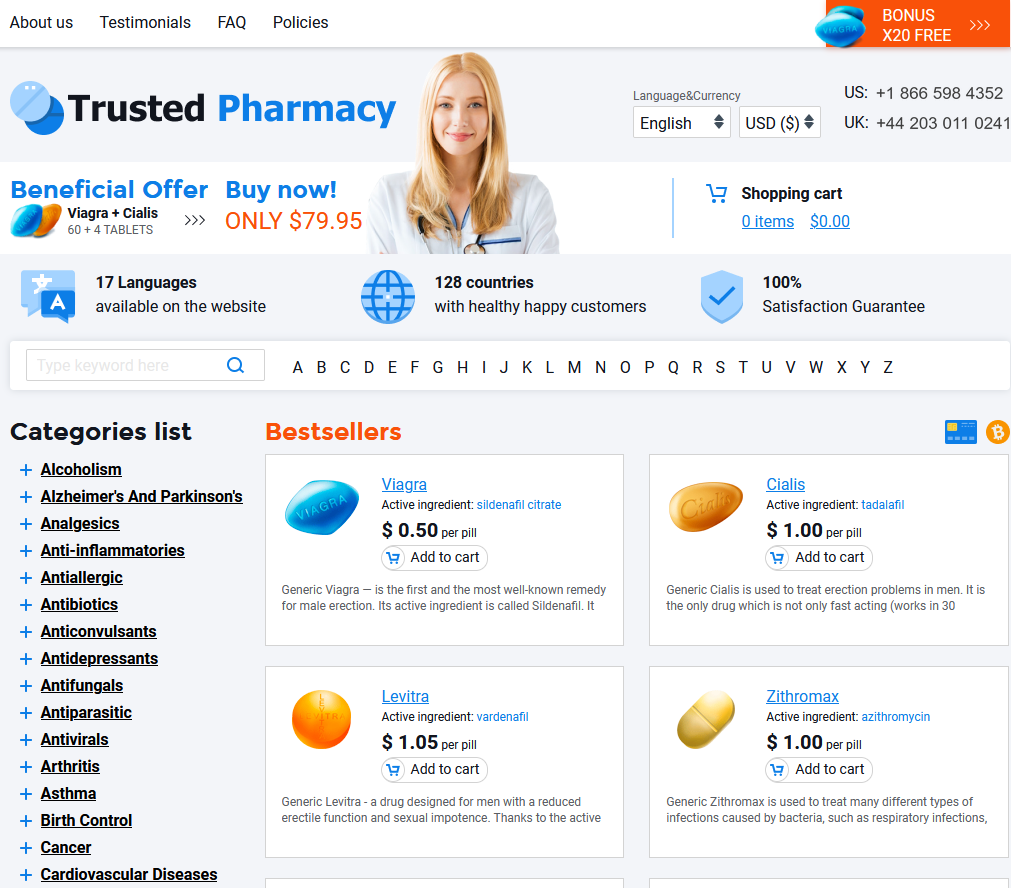
To Buy Azithromycin Online Visit Our Pharmacy ↓
 The Impact of Azithromycin on Common Respiratory Infections
The Impact of Azithromycin on Common Respiratory Infections
Azithromycin, a macrolide antibiotic, is appreciated for its broad-spectrum activity and unique pharmacokinetics. Originally derived from erythromycin, it boasts a modified lactone ring structure that confers increased acid stability and enhanced tissue penetration. Notably, its ability to accumulate within cells, particularly in phagocytes, allows it to be delivered directly to the site of infection. This property also underpins its extended half-life, which enables shorter and less frequent dosing regimens compared to many other antibiotics.
Delving deeper, what sets azithromycin apart is its mechanism of action. It inhibits bacterial protein synthesis by binding to the 50S subunit of the bacterial ribosome, thus halting the growth of the bacteria. This specific action contributes to its effectiveness against a variety of respiratory pathogens. Moreover, its anti-inflammatory properties have been observed in several studies, making it an interesting subject for research beyond its antimicrobial usage, with potential implications for treating chronic inflammatory respiratory diseases.
The Battle Against Bacteria in Respiratory Infections
Respiratory infections, ranging from the common cold to more severe illnesses like pneumonia, are predominantly caused by a myriad of bacteria and viruses. Azithromycin, a broad-spectrum antibiotic, is particularly effective against a variety of bacteria responsible for these infections. Its mode of action involves inhibiting bacterial protein synthesis by binding to the 50S ribosomal subunit, ultimately preventing the bacteria from growing and spreading. The effectiveness of azithromycin is most notable in the treatment of infections caused by Streptococcus pneumoniae and Haemophilus influenzae, common culprits behind bacterial respiratory ailments.
While viruses also play a significant role in respiratory infections, antibiotics like azithromycin have no effect on them. Nonetheless, clinicians often prescribe azithromycin for bacterial superinfections that can complicate the course of viral illnesses, such as influenza. The antibiotic's prolonged half-life allows for a shorter course of therapy, usually five days, which contributes to patient adherence and satisfaction. However, its indiscretion use for viral infections can contribute to bacterial resistance, an emerging concern in the battle against respiratory infections.
Azithromycin's Role in Treating Pneumonia and Bronchitis
Azithromycin, a broad-spectrum antibiotic, is commonly prescribed to combat respiratory infections like pneumonia and bronchitis due to its effectiveness against a wide range of bacteria. For pneumonia, it has been a go-to treatment, especially for atypical organisms and in community-acquired cases where it's favored for its high intra-tissue concentrations and long half-life allowing for shorter and more convenient treatment regimens. Its anti-inflammatory properties also offer additional benefits, potentially reducing the severity of symptoms and the risk of complications.
In cases of acute bronchitis, azithromycin's role is more nuanced. While viral infections are the primary cause and antibiotics are generally not recommended, it is used when bacterial infection is suspected or there's a high risk of secondary bacterial infection. The medication's once-daily dosing and short course therapy are advantageous for patient adherence, which is critical for effective treatment and recovery. Careful diagnostic efforts are necessary to ensure its appropriate use, helping to mitigate the development of antibiotic resistance.
Understanding Resistance: the Downside of Overuse
Azithromycin, like all antibiotics, is not without its pitfalls. Chief among them is the development of antibiotic resistance, which is a direct consequence of antibiotic overuse and misuse. When azithromycin is unnecessarily prescribed or not taken as directed, bacteria can adapt and become resistant to the drug, rendering it less effective. This resistance can spread among bacterial populations, leading to a public health challenge where common therapies no longer work against once-treatable infections.
The evolution of resistant strains means that some patients may face longer illnesses, more severe symptoms, or have fewer treatment options available. The medical community is increasingly cautious about prescribing antibiotics like azithromycin without clear bacterial indications. Healthcare providers are urged to follow strict guidelines when it comes to antibiotic prescriptions, and patients are reminded of the importance of taking the full course of antibiotics as prescribed to help mitigate the rise in resistant infections.
Comparing Azithromycin with Other Antibiotics
Azithromycin stands out due to its unique pharmacokinetics, presenting an advantage over other antibiotics like amoxicillin and doxycycline, typically requiring a more frequent dosage. With a long half-life, azithromycin allows for a short course therapy, often completed within five days, which can improve patient compliance. The drug accumulates effectively in tissues, particularly those of the respiratory tract, resulting in sustained antibacterial activity. Its once-daily dosing contrasts with the thrice or four times a day regimen required for many penicillins and cephalosporins, which can be more disruptive to a patient's daily routine and may contribute to missed doses and subsequent treatment failure.
Nevertheless, there are scenarios where azithromycin isn't the first-line choice due to resistance patterns or specific bacterial etiologies. For example, amoxicillin-clavulanate might be preferred in acute bacterial sinusitis owing to its broad spectrum of activity against common pathogens, including those that produce beta-lactamase. In treating streptococcal pharyngitis, penicillin remains the antibiotic of choice due to its efficacy, safety profile, and narrow spectrum, which minimizes disruption to the commensal flora and the risk of resistance development. Tailoring antibiotic selection to the suspected or confirmed pathogen, local resistance patterns, and individual patient characteristics is key to maximizing therapeutic success.
Patient Experiences: Real-life Stories of Recovery
The emotional weight of battling a respiratory infection can be quite significant, but the relief that comes with effective treatment is often deeply felt. Azithromycin, known for its ease of use and quick action, has become a beacon of hope for many. One such story involves a school teacher who, after weeks of fruitless treatment with other medications, found solace in azithromycin. Despite facing a severe bout of bronchitis that had her missing classes and feeling despondent, this antibiotic turned the tide, facilitating a swift recovery that allowed her to return to the classroom with renewed vigor and health.
On the more severe end of the spectrum, azithromycin has played a pivotal role for patients grappling with pneumonia. An elderly patient's journey to recovery illustrates the drug's efficacy; fighting a persistent lung infection that seemed to resist initial treatments, the introduction of azithromycin was a turning point. Within days, symptoms that had caused distress and prompted hospital visits began to subside, leading to a complete recovery that her family described as nothing short of miraculous. These personal accounts not only underscore the drug's potential for healing but also emphasize the profound impact that the right antibiotic therapy can have on individuals’ lives.
